| To advance
and promote the discipline and professional practice of epidemiology in
Ontario public health units |
 |
| Please click here to visit our new website |

|


 |
| 6B Neonatal and Infant Mortality Rates |
Description | Specific Indicators | Ontario Public Health Standards | Corresponding Health Indicators(s) from Statistics Canada and CIHI | Corresponding Indicators(s) from Other Sources| Data Sources | Alternative Data Sources | ICD Codes | Analysis Check List | Method of Calculation | Basic Categories | Indicator Comments | Definitions | Cross-References to Other Indicators| Cited References | Changes Made | Acknowledgements | Description | - The ratio of the number of deaths of live born infants during a calendar year per 1,000 live births in the same calendar year.
|
Specific Indicators | Neonatal mortality rate - Post-neonatal mortality rate
- Infant mortality rate (IMR)
| | Ontario Public Health Standards (OPHS) | The Ontario Public Health Standards (OPHS) establish requirements for the fundamental public health programs and services carried out by boards of health, which include assessment and surveillance, health promotion and policy development, disease and injury prevention, and health protection. The OPHS consist of one Foundational Standard and 13 Program Standards that articulate broad societal goals that result from the activities undertaken by boards of health and many others, including community partners, non-governmental organizations, and governmental bodies. These results have been expressed in terms of two levels of outcomes: societal outcomes and board of health outcomes. Societal outcomes entail changes in health status, organizations, systems, norms, policies, environments, and practices and result from the work of many sectors of society, including boards of health, for the improvement of the overall health of the population. Board of health outcomes are the results of endeavours by boards of health and often focus on changes in awareness, knowledge, attitudes, skills, practices, environments, and policies. Boards of health are accountable for these outcomes. The standards also outline the requirements that boards of health must implement to achieve the stated results. | | Outcomes Related to this Indicator | - Board of Health Outcome (Reproductive Health): The board of health is aware of and uses epidemiology to influence the development of healthy public policy and its programs and services for the promotion of reproductive health.
- Board of Health Outcome (Foundational Standard): The public, community partners, and health care providers are aware of relevant and current population health information Assessment and/or Surveillance Requirements Related to this Indicator.
| | Assessment and Surveillance Requirements Related to this Indicator (Reproductive Health) | - The board of health shall conduct epidemiological analysis of surveillance data... in the area of reproductive health outcomes.
| http://www.ontario.ca/publichealthstandards
| | Corresponding Health Indicator(s) from Statistics Canada and CIHI | - Infant Mortality Rates (IMR)
This indicator includes all infant deaths and live births (including those weighing <500g) occurring within a given calendar year. Annual IMRs are available through CANSIM from 1974 to most recent available year, nationally and by province/territory. Annual rates are available by age at time of death (under 1 year (infant mortality), 0-27 days (neonatal), 28-364 days (postneonatal), under 1 day, 1-6 days, 7-27 days, 1-2 months, 3-5 months, 6-11 months). http://www.statcan.gc.ca/pub/82-221-x/82-221-x2011002-eng.htm Click on "data tables, maps and fact sheets" on menu on left side of page
Click on "Infant Mortality" under "Health Status", "Deaths | | Corresponding Indicator(s) from Other Sources |
World Health Organization (WHO)
| - Neonatal Mortality Rate (0-27 days) and Infant Mortality Rate (0-364 days)
Under "World Health Statistics" - "Mortality and burden of disease" - "Child Mortality" http://apps.who.int/ghodata/ These rates are adjusted estimates produced for the United Nations by the Inter-agency Group for Mortality Estimation (IGME) and are not necessarily the same as official national statistics. For detailed indicator definition, see the latest World Health Statistics Indicators Compendium. | | Canadian Perinatal Surveillance System (CPSS), Public Health Agency of Canada | Infant Mortality Rate (0-364 days) Neonatal Mortality Rate (0-27 days) Post-neonatal Mortality Rate (28-364 days)
Latest statistics are reported in the Canadian Perinatal Health Report: 2008 Edition (1). PHAC reports IMRs, neonatal mortality rates and post-neonatal mortality rates in two ways: as a period infant mortality rate (includes all births and all infant deaths occurring in a given calendar year) and as a birth cohort mortality rate (based on births (≥500g) occurring in a calendar year, whether or not the resulting infant death occurred in the same or following year). Note that Ontario data were excluded from most analyses throughout their 2008 report due to data quality concerns (1). | | Data Sources (see Resources: Data Sources) | Numerator: Vital Statistics - Mortality Data
Original source: Vital Statistics, Ontario Office of the Registrar General (ORG)
Distributed by: Ontario Ministry of Health and Long-Term Care (MOHLTC): IntelliHEALTH Ontario (IntelliHEALTH)
Suggested citation (see Data Citation Notes): Ontario Mortality Data [years], Ontario Ministry of Health and Long-Term Care, IntelliHEALTH ONTARIO, Date Extracted: [date].
Denominator: Vital Statistics - Live Birth Data
Original source: Vital Statistics, Office of the Registrar General (ORG)
Distributed by: Ontario Ministry of Health and Long-Term Care (MOHLTC): IntelliHEALTH ONTARIO (IntelliHEALTH)
Suggested citation (see Data Citation Notes): Ontario Live Birth Data [years], Ontario Ministry of Health and Long-Term Care, IntelliHEALTH ONTARIO, Date Extracted: [date]. | | Alternative Data Source(s) | | | ICD Codes | All causes - All accidental deaths (ICD-9: E800-E999); (ICD-10-CA: V01-Z99)
- Homicide/infanticide (ICD-9: E960-E969); (ICD-10-CA: X85-Y09)
- Shaken Baby Syndrome (ICD-9: 850-854 with E967); (ICD-10-CA: S06 with Y07)
- Child battery and maltreatment or criminal neglect (ICD-9: E967 & E968.4); (ICD-10-CA: Y06-Y07)
- Falls (ICD-9: E880-E888); (ICD-10-CA: W00-W19)
- RDS: Respiratory Distress Syndrome (ICD-9: 769.0-769.9); (ICD-10-CA: P22)
- SIDS: Sudden Infant Death Syndrome (ICD-9: 798.0); (ICD-10-CA: R95)
- Congenital anomalies (ICD-9: 740-759); (ICD-10-CA: Q00-Q99)
- Low birth weight (not short gestation) (ICD-9: 764); (ICD-10-CA: P05)
- Low birth weight with short gestation (ICD-9: 765); (ICD-10-CA: P07)
- Intrauterine hypoxia and birth asphyxia (ICD-9: 768); (ICD-10-CA: P20 & P21)
- Other conditions of the perinatal period (ICD-9: 760-764, 766, & 770-779); (ICD-10-CA: P00-P04, P08, & P23-P96)
- Pneumonia and influenza (ICD-9: 480-487); (ICD-10-CA: J10-J18)
- Certain gastrointestinal diseases (ICD-9: 008-009, 535, & 555-558); (ICD-10-CA: A00-A09, K29, K50-K52, K55-K63)
| | Analysis Check List | - The IntelliHEALTH licensing agreement does not require suppression of small cells, but caution should be used when reporting at a level that could identify individuals, (e.g. reporting at the postal code level by age and sex). Please note that privacy policies may vary by organization. Prior to releasing data, ensure adherence to the privacy policy of your organization.
- Aggregation (e.g. combining years, age groups, categories) should also be considered when small numbers result in unstable rates.
- Analyze by infant residence, not place of death.
- Some authors suggest a denominator of 10,000 or more to obtain accurate estimates of mortality.
- Small numbers of events may require the suppression of information, collapsing several years of data, or the use of smoothing techniques to eliminate large variations in reported rates.
- HELPS Data: Historically, PHUs obtained data for live births, stillbirths, therapeutic abortions, congenital anomalies, and deaths from the Ministry of Health through HELPS (the HEalthPlanning System). Although these data are no longer commonly used, some PHUs may still be accessing these data files. Information about the data can be found in the HELPS Data Source resource.
| | Vital Statistics Mortality Data | - Use Deaths data source from the Vital Statistics folder in Intellihealth, select # ON Deaths measure (number of deaths for Ontario residents who died in Ontario). Note: deaths for Ontario residents who died outside the province are not captured in Vital Statistics.
- Select appropriate geography from Deceased Information folder. Include other items, depending on your requirements (ICD10 Chapter, Lead Cause Group, age group, sex, etc.).
- In the mortality data set, External Cause of Injury Codes (ICD10 V-Y; ICD9 E-Codes), and not Injury & Poisoning Codes (ICD10 S-T codes; ICD9 800-999 codes) are used in assigning primary cause of death.
| | Vital Statistics Live Birth Data | - In IntelliHEALTH under Standard Reports, folder "01 Vital Stats", open " Birth Summary V2". This report summarizes information on births by age group and mother's residence (Ontario, PHU and LHIN). IntelliHEALTH also provides population data (total population, female population aged 15-49 years) for the calculation of rates. Refer to the Notes tab for information. Open tab "1.2 Births x PHU x Type x Age" to obtain public health unit data and tab "1.1 ON Births x Type x Age" to obtain Ontario data. The report can be modified, renamed and saved under your own folder or can be exported into Excel.
- The predefined report provides live birth and population data for the calendar years from 2000 to the most recent available. Table options can be edited to change the number of years of data presented. For years that are not displayed modify the calendar year filter to include the required years.
- The data contained in the Birth Summary V2 report includes birth to Ontario mothers in Ontario only.
- The notes section of the report provides important data caveats and background information on data sources and should be consulted.
| Method of Calculation
| | Infant Mortality Rate | total number of deaths for live born infants (364 days or younger) | x 1,000 |
| total number of live births |
Neonatal Mortality Rate | total number of deaths for live born infants (27 days or younger) | x 1,000 |
| total number of live births |
Post-Neonatal Mortality Rate | total number of deaths for live born infants (28-364 days) | x 1,000 |
| total number of live births |
| | Basic Categories | Geographic areas of patient residence: Ontario, public health unit, municipality, and smaller areas of geography based on aggregated postal code. Age of mother, gestational age, birth weight, sex of infant - Age of infant (early neonatal: 0-6 days, late neonatal: 7-27 days, or post-neonatal: 28-364 days)
| | Indicator Comments | Infant mortality rates are considered an indicator of social and economic conditions within a country, community or subpopulation (2, 3). High rates may reflect inadequate nutrition, low levels of education, exposure to environmental hazards, limited utilization of or access to adequate health care services (3). - Infant mortality rates may vary by country due to the definition of a live birth.
- Disparities in the risk of infant death across subpopulations have been reported previously in Canada (including aboriginal populations) (4, 5).
- In 1999, congenital anomalies were the leading cause of infant death in Canada; however immaturity became the leading cause of infant death in 2004. Immaturity was the leading cause of neonatal death, and congenital anomalies was the leading cause of post-neonatal death in Canada in 2004 (1).
- Determining the true cause of death is not always clear resulting in somewhat subjective primary cause of death being listed on death certificate. The reported cause of death may also be influenced by the social or legal conditions surrounding the death and by the level of medical investigation.
- Registration fees initiated in some CSDs in 1996 may have reduced the number of infants registered, especially for low income and/or adolescent parents (6); however it is worth noting that registration fees have since been discontinued in Ontario. Please refer to the Timeline of changes in Live Birth Registration in Ontario document for details.
- In all provinces except Ontario, Statistics Canada linkages of live birth and infant death registration are successful for all but 1.1% of cases (2003); in Ontario 42.3% were unlinked (1). The unlinked cases vary from linked cases by time of death and cause of death (1). This linkage issue precludes the reliable calculation certain figures, such as gestational age-specific infant mortality rates.
- Infant mortality rates are higher among multiple births (8) and births to mothers over 35 (9). Changing pattern of registration of live births with a birth weight less than 500 grams in Canada has shown to have significantly increased infant mortality rates as such infants have very high rates of mortality (10).
- It is recommended to exclude births weighing <500 g from neonatal and infant mortality rates. Doing so may reduce fluctuations in estimates and facilitate comparisons across jurisdictions. However, it is not possible to examine neonatal and infant mortality among births ≥500 g due to data limitations in Ontario. Please refer to the Reproductive Health Core Indicators Documentation Report for recommendations on excluding live births <500 g from reproductive health indicators.
- Given the small number of stillbirths/perinatal/infant deaths, stillbirth rate, perinatal/infant mortality rates may fluctuate from year to year. It may be of beneficial to group years when reporting stillbirth rate/perinatal mortality/infant mortality and/or calculate a three-year moving average (Refer to Document: Methods for Calculating Moving Averages).
- ICD code groupings provided in the Canadian Perinatal Health Report (appendix A.2) may be useful if choosing to examine infant mortality by cause (1).
- Neither BORN nor Hospitalization birth records can be linked to vital statistics mortality data at this time. Therefore, BORN and Hospitalization data sources cannot be used to determine neonatal or infant mortality.
| | Definitions | - Live birth - the complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of the pregnancy, which, after such separation, breathes or shows any other evidence of life such as heartbeat, umbilical cord pulsation, or definite movement of voluntary muscles, whether the umbilical cord has been cut or the placenta is attached. A live birth is not necessarily a viable birth.
- Infant mortality - death of a live born infant before the 365th day of life.
- Mortality rates - based on deaths during the following specified periods:
- Infancy (infant) - the period between a live birth and 364 days of life.
- Late neonatal - the period between the 7th and 27th day of life.
- Neonatal - the period life between a live birth and the 27th day of life.
- Post-neonatal - the death of a live born infant between the 28th and 364th day of life.
- Sudden infant death syndrome (SIDS) - the unexpected and sudden death of an apparently healthy infant. It is more often reported in infants between two weeks and one year of age, in preterm infants, and males. Also called crib death. ICD-9 code: 798.0. Note that some researchers use ICD-9 codes: 798.0-798.9.
- Respiratory distress syndrome (RDS) - a respiratory disorder that occurs in newborn premature infants and is characterized by deficiency of the surfactant coating the inner surface of the lungs, failure of the lungs to expand and contract properly during breathing resulting in collapse; and by the accumulation of a protein-containing film lining the alveoli and their ducts. Also called hyaline membrane disease;
- Congenital anomaly - a condition that results from an abnormality of structure, function or metabolism in one or more parts of the body, with potential to adversely affect health, development or function. Anomalies are present at birth and may be inherited genetically, acquired during gestation, or inflicted during birth. Also called a birth defect.
- Intrauterine Hypoxia (IH) - occurs when the fetus is deprived of an adequate supply of oxygen. IH is used to describe inadequate oxygen availability during the gestation period.
- Birth asphyxia - (also refered to as perinatal asphyxia or Asphyxia neonatorum ) can result from inadequate supply of oxygen immediately prior to, during or just after delivery.
| Components of Fetal-Infant Mortality | 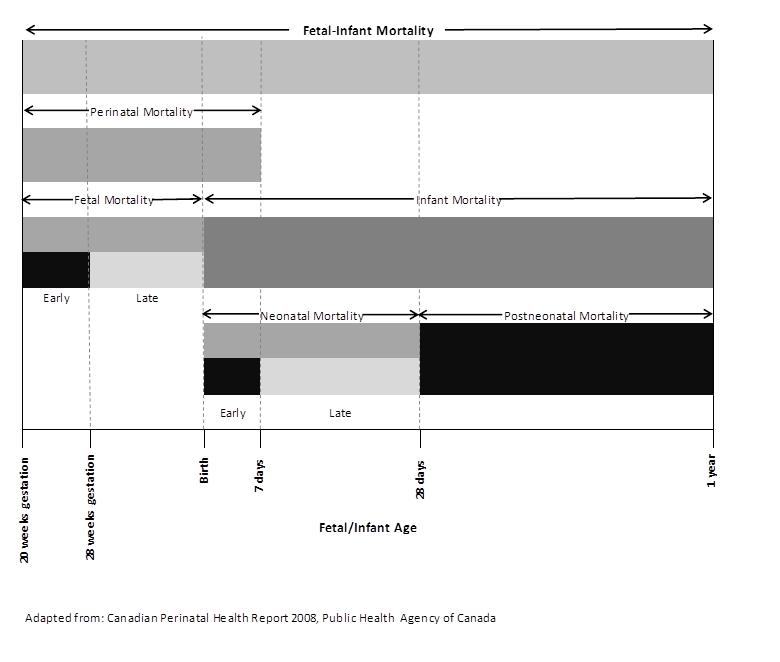
| | Cross-References to Other Indicators | | | Cited References | - World Health Organization. Neonatal and perinatal mortality: Country, regional, global estimates. Geneva, 2006. Available from: http://whqlibdoc.who.int/publications/2006/9241563206_eng.pdf
- Spong, CY, Iams, J, Goldenberg, R. Hauck, FR, Willinger, M. Disparities in perinatal medicine. Obstet Gynecol. 2011;117(4):948-955.
- Kleinman JC. The slowdown in the infant mortality decline. Paediatric Perinatal Epidemiology. 1990; 4(4):373-381.
- Luo ZC, Senecal S, Simonet F, Guimond E, Penney C, Wilkins, R. Birth outcomes in the Inuit-inhabited areas of Canada. Canadian Medical Association Journal 2010, 182(3): 235-42
- Bienefeld M, Woodward GL, Ardal S. Underreporting of live births in Ontario: 1991-1997. Central East Health Information Partnership, February 2001.
- Woodward GL, Ardal S. Data Quality Report: Effect of Residence Code Errors on Fertility Rates. Central East Health Information Partnership, July 2000.
- Mathews TJ, MacDorman MF. Infant mortality statistics from the 2007 period linked birth/infant death data set. National Vital Statistics Report (US). 2011 June 29; 59(6):1-31.
- Gage TB, Fang F, O'Neill E, Stratton H. Maternal age and infant mortality: a test of the Wilcox-Russell hypothesis. American Journal of Epidemiology 2009; 169(3):294-303.
- Joseph KS, Kramer MS. Recent trends in Canadian infant mortality rates: the effect of changes in registration of live newborns weighing less than 500g. Can Med Assoc J 1996; 155(4):1047-52.
| | Changes Made | Date | Type of Review-Formal Review or Ad Hoc? | Changes made by | Changes | May 30, 2005 | | | | March 29, 2012 - January 16, 2013 | Formal Review | Reproductive Health Sub-Group | - All sections updated in alignment with the Guide to Creating or Editing Core Indicator pages
- Significant changes made to many aspects of indicator, including: Specific Indicators, Corresponding Indicators from Other Sources, Data Sources, Method of Calculation, Definitions, Indicator Comments, Cited References, Other References.
|
| | Acknowledgements | Lead Author(s) | - Jessica Deming, Region of Waterloo Public Health
- Sandy Dupuis, Niagara Region Public Health
- Natalie Greenidge, Public Health Ontario
| Contributing Authors(s) | - Reproductive Health Sub-group
| Reviewers | - Ahalya Mahendra, Public Health Agency of Canada (Reproductive Health Core Indicators Work Group Member)
- Carmen Yue, Toronto Public Health
|
|
|
|
|
|
|